A 36 year old male with vomiting and pain abdomen
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 36 year old male, shop keeper by occupation, resident of Kolkata, West Bengal, came to OPD with chief complaints of vomiting since 2 months and pain in the abdomen since 2 months.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 months ago and then he developed vomiting which was insidious in onset, gradually progressive. The content of vomiting was food particles, yellow to green in color (non bilious), non projectile vomiting, no relation to pain. He had 4-5 episodes per day, occurs two to three hours after taking a meal. It occurs with both liquids and solids. It is associated with nausea, giddiness, constipation, belching, regurgitation. Appetite was normal. Aggravated on taking food and no relieving factors. Patient also complained of pain abdomen which was insidious in onset, non progressive, no radiation of pain. It was squeezing type and diffuse. There are no aggravating and relieving factors.
History of lethargy and weight loss. History of jaundice which was diagnosed incidently 2 months ago and visited a hospital in West bengal but no relief despite medications.
No history of dysphagia, odynophagia, heartburn, indigestion, flatulence, diarrhoea, abdominal distention, hematemesis, melaena, urinary symptoms, chest pain, cold, cough.
Endoscopy was done in April outside hospital in Behar and was diagnosed as esophageal candidiasis, Lax LES, Pangastritis, Duodenitis.
DAILY ROUTINE:
Patient wakes up around 6 in the morning and freshens up. Has his breakfast and goes to work where he is a shopkeeper . Takes his lunch during work and comes back home around 9 and takes his dinner.
PAST HISTORY:
Patient had no similar complaints in the past.
Not a known case of Hypertension, Diabetes, CAD, Epilepsy, TB, Thyroid disorders.
FAMILY HISTORY:
No similar complaints seen in the family.
PERSONAL HISTORY:
Diet is mixed, appetite is normal, sleep inadequate since 2 months due to pain, bladder movements are regular, bowel movements- constipation since 2 months. History of weight loss since 2 months. Patient takes khaini since teenage. Patient is a non smoker, does not consume alcohol, chew tobacco etc. No known allergies. Not any kind of medication.
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative, well oriented to time, place and person. Thin built and poorly nourished.
Patient has pallor. No signs of icterus, cyanosis, clubbing, lymphadenopathy and edema.
Vitals: Temp: afebrile PR: 70/min RR: 16cpm BP: 90/60mmHg SpO2: 98%
SYSTEMIC EXAMINATION:
Per abdomen:
On Inspection, shape of abdomen is flat, no flank fullness, Umblicus is centrally placed and inverted. Movements of abdominal wall are normal. Skin over abdomen is normal. No pigmentation seen, No sinuses, scars, dilated veins, visible pulsations and hernial orifices.
On Palpation, all inspectory findings are confirmed. No local rise of temperature. No tenderness is seen. Palpable mass in right hypocondrial region. Liver and spleen are not palpable. Kidney not palpable.
On Percussion, no fluid thrill or shifting dullness.
On Auscultation, bowel sounds are reduced (4/min heard).
CVS: S1, S2 heard. No murmurs, thrills, heeves.
Resp: BAE + NVBS +
CNS: No neurological focal deficits are seen.
PROVISIONAL DIAGNOSIS:
Subacute obstruction..? Chronic ulcer lead to inflammatory reaction and ? fibrosis
Infective ( Abdominal TB )
Inflammatory corns,ulcers
Malignancy
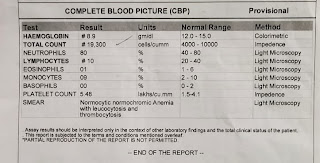
INVESTIGATIONS:
Previous hospital records during April,May
Shows dialated bowl loops
TREATMENT:
1. TAB. RAZO 40mg OD
2. Monitor vitals 6th hourly.
















Comments
Post a Comment